Burnout and post-traumatic stress disorder (PTSD) rates are soaring across healthcare as we enter the pandemic’s fourth wave and move closer to year three. While all that provide healthcare are profoundly affected by the amount and level of care needed, stress levels are incredibly high for those on the frontlines in emergency medicine, where emergency departments (ED) once again have become overwhelmed with Covid-19 patients.
Emergency care hard hit by PTSD
PTSD statistics are particularly problematic. An American Nurses Foundation survey examined the impact of Covid-19 on nurses’ mental wellbeing, including 442 ED nurses. Conducted in December 2020, the survey found that in the previous 14 days, ED nurses reported feeling exhausted (81%), overwhelmed (67%), anxious or unable to relax (64%), depressed (44%), and angry (43%). Only 33% had confidence in their “ability to handle things.” ED nurses had higher percentages in nearly all of these areas than the broader population of 12,418 nurses who participated in the study.
Physicians are just as stressed. A survey published in the Journal of the American College of Emergency Physicians found that 22% of 1,300 emergency physicians “reported symptoms of stress consistent with PTSD” during Covid. Another study presented at the American Psychiatric Association annual meeting in May 2021 found that 36% of 1,390 physicians with no active history of PTSD had PTSD during the pandemic.
This critical clinical situation is hitting against a backdrop of pent-up frustration among clinicians who must deal with increasing performance measures and an electronic health record (EHR) that is becoming more complex—just a few areas that add stress and take crucial time away from patient care.
Emergency Department clinicians are well-trained to handle trauma and are used to working in fast-paced, high-stress environments in which they can expect to treat multiple trauma patients and may see a high rate of fatalities during a single shift. Stress in trauma care happens relatively fast, however, and then it is over, unlike the sustained stress or personal risk brought on by Covid-19. Stress levels can elevate even more quickly when treating a Covid patient because there remain many unknowns around treatment and outcomes.
The pandemic is an entirely different type of stress in that it affects every human being. It is a prolonged source of stress with no end in sight and limited safe zones. At the start of the pandemic, clinicians were forced to quickly learn and adapt to new assessment and care rules and sort through treatment options while facing a completely unknown clinical pathway and prognosis. While much has been learned, the new Delta variant starts it all again, while dealing with the realistic concern that they may contract the virus or asymptomatically share it with their family.
This is happening across all inpatient environments. For example, when floor nurses, who are used to caring for stable patients, were put on Covid-19 units or in the ICU where the patient didn’t have family support, not only did they have to take care of very sick patients at significant risk to themselves, but they also had the burden of providing emotional support. That is tremendously stressful for clinicians. The outcome is that 30% of healthcare workers are considering leaving the profession, according to a 2021 Washington Post/Kaiser Family Foundation survey.
How technology can reduce clinical workflow burdens
As cases have spiked in the face of the Delta variant and a watchful eye is on the Lambda variant, we face the real possibility of the virus becoming endemic and, thus, a long-term event for clinicians on the front lines and everywhere. The additional, cumulative effect for clinicians who already work in high-stress areas such as emergency medicine is worrisome. While the healthcare workforce has more mental health services available to them than ever before, including resilience awareness and training, it’s essential to find other ways to help reduce clinician stress, burnout, and PTSD.
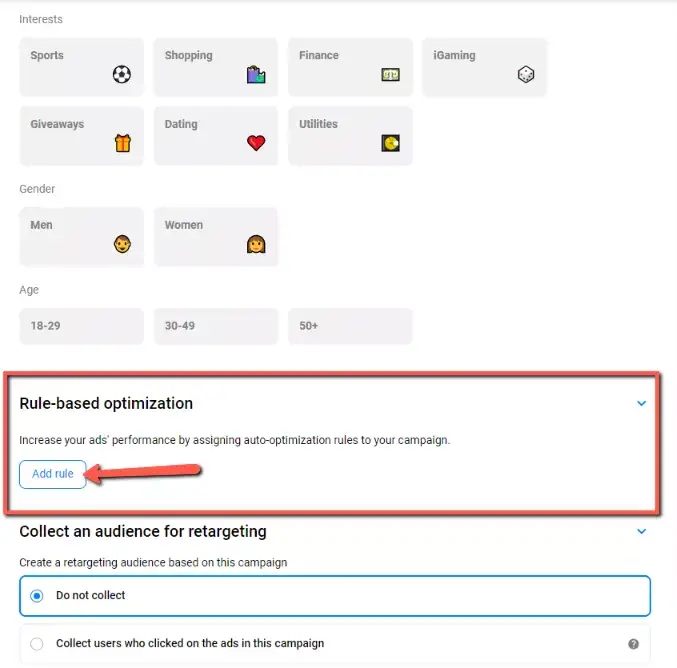
One goal is to develop and provide beneficial technology that can help offload the manual work away from bedside care. As clinicians take on the important job of supporting patients through this devastating illness, it is increasingly important for healthcare leaders to provide clinical teams with supportive technology.
Technology can do a better job of supporting human connections between clinicians and patients. Nurses can gain some relief by offloading tasks that a software program can handle. (For example, during the pandemic, nurses were often put on different floors and into new situations where they didn’t know anyone, which became problematic when they had to call another clinician for help. Looking up phone numbers was time-consuming. In this situation, voice technology, for example, can help a nurse find help more quickly by allowing the person to call out a job role. Saratoga Hospital has already implemented this type of technology in their ICU, improving communication and safety while also conserving PPE during the pandemic.
If ED patients need additional care, ED nurses move patients to the right clinical environment. During pandemic surges, arranging clinical transport for one patient can now take as many as 150 calls, according to our data. This adds patient placement and bed availability to the Covid-19 processes and providing the clinical and emotional needs that come with caring for a sick patient. Patient movement technology can offload this work by taking over numerous logistical processes. These types of technology solutions not only take over manual work that is easily automated, but they also give clinicians another vitally needed layer of support, reducing their isolation during stressful and difficult times.
As the Delta variant surges on, we understand trauma for healthcare providers isn’t over, but we are hopeful technology can make a small impact in lightening the load for our front-line heroes.
Photo: Ivan-balvan, Getty Images